Vaginal Prolapse: Understanding Your Condition
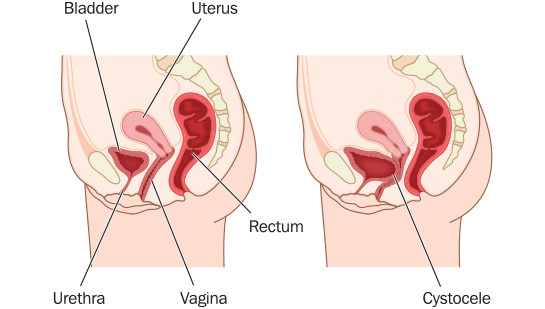
Vaginal prolapse is a condition in which structures such as the bladder, rectum, urethra, uterus, small bowel or the vagina itself may begin to prolapse, or fall out of their normal positions. If the patient doesn’t seek medical treatment or surgery, these structures may eventually prolapse farther into the vagina or even through the vaginal opening if their supports weaken enough.
The issues that arise from vaginal prolapse commonly affect sexual function as well as normal bodily functions such as urination and defecation. Pelvic pressure and discomfort are also common indicators of vaginal prolapse.
Symptoms of Vaginal Prolapse:
The symptoms generally associated with vaginal prolapse depend on the type of vaginal prolapse present. The most common symptom of all types of vaginal prolapse is the sensation that tissues or structures in the vagina feel out of place. This may involve a protrusion or pressure in the area of the sensation. Other common symptoms include:
- Pressure in the vagina or pelvis
- Painful intercourse
- A mass at the opening of the vagina
- A decrease in pain or pressure when the woman lies down
- Recurrent urinary tract infections
- Difficulty emptying the bowl or bladder
- Constipation
- Urinary stress incontinence
- Pain that increases during long periods of standing
- Enlarged, wide, and gaping vaginal opening
Causes for Vaginal Prolapse:
A vaginal prolapse occurs when the weight-bearing or stabilizing structures that keep the vagina in place weaken or deteriorate. This may cause the supports for the rectum, bladder, uterus, small bladder, urethra, or a combination of them to become less stable. Common factors that may cause a vaginal prolapse include the following:
- Childbirth (especially large babies)
- Menopause
- Hysterectomy
- Advanced age
- Obesity
- Dysfunction of the nerves and tissues
- Abnormalities of the connective tissue
- Strenuous physical activity
- Prior pelvic surgery
Tests Used for Diagnosing Vaginal Prolapse:
In most cases, the most reliable way for your physician to make a confident diagnosis of any type of vaginal prolapse involves a medical history and a thorough physical examination. Other diagnostic tests may include:
- Q-tip test – the doctor inserts a small cotton-tipped applicator into the woman’s urethra. The doctor then asks the woman to strain down. If the applicator raises 30 degrees or more as a result, this means that the urethra descends while straining and is a predictive factor of success of anti-incontinence surgery.
- Bladder function test – this tests the ability of the bladder to store and evacuate urine and to dispose of it. This is important clinical information that may assist the surgeon in selecting the correct type of surgery.
- Pelvic floor strength – during the pelvic examination, the doctor tests the strength of the woman’s pelvic floor and of her sphincter muscles. The doctor also assesses the strength of the muscles and ligaments that support the vaginal walls, uterus, rectum, urethra, and bladder.
- Ultrasound- used to evaluate the muscles of the pelvic floor
- MRI – This large machine uses a magnet linked to a computer to create detailed pictures of your urinary tract and lymph nodes. An MRI can show cancer in your kidneys, lymph nodes or other tissues in the abdomen.
Treatment Options for Vaginal Prolapse:
Treatment of vaginal prolapse is different for every patient depending on the organs involved, how bad the symptoms are, and what other medical conditions are present. Vaginal prolapse can be a long-lasting condition, but some women are able to relieve or lessen their symptoms without treatment by adjusting their activities and lifestyle habits. These changes may include:
- Performing Kegel exercises daily to tighten and strengthen pelvic muscles.
- Avoiding activities that stress your pelvic muscles, such as heavy lifting.
If your symptoms are not relieved by these lifestyle changes, you may need more advanced treatment including:
- Cystocele or Urethrocele – repair of the bladder or urethra
- Hysterectomy – removal of the uterus
- Rectocele or Enterocele – repair of the rectum or small bowel
- Vaginal Vault Suspension – repair of the vaginal wall
- Vaginal Obliteration – closure of the vagina
While vaginal prolapse is fairly common, it can be embarrassing and frustrating for you as the patient. We at Western Michigan Urological Associates can help alleviate immediate pain and help you develop a plan to improve your quality of life and alleviate symptoms of pelvic floor dysfunction. Ask Your Primary Care Provider for a Referral.
Vaginal Prolapse
Most women develop some form of vaginal prolapse during their lifetime.
Women’s Urologic Conditions
See statistics on women-specific conditions including incontinence, UTIs, organ prolapse and more.
Incontinence Do You Call It Voiding …or Embarrassing?
Don’t let your incontinence get in the way of your life any longer. Help is just around the corner.